The Hormone-Immune Axis: An Overlooked Driver of Autoimmune Vulnerability
Nearly 80% of people with an autoimmune disease are women. This striking statistic underscores the need to examine the potential connection between hormone imbalance and immune dysfunction in women. Hormones and the immune system are in constant cross-talk, influencing each other in ways that can either support or sabotage immune tolerance.
When hormone balance falters—due to menstrual fluctuations, chronic stress, or thyroid dysfunction—immune regulation can unravel. At the same time, immune activation and cytokine release can disrupt hormone production and receptor sensitivity, creating a feedback loop that drives inflammation and autoimmunity.
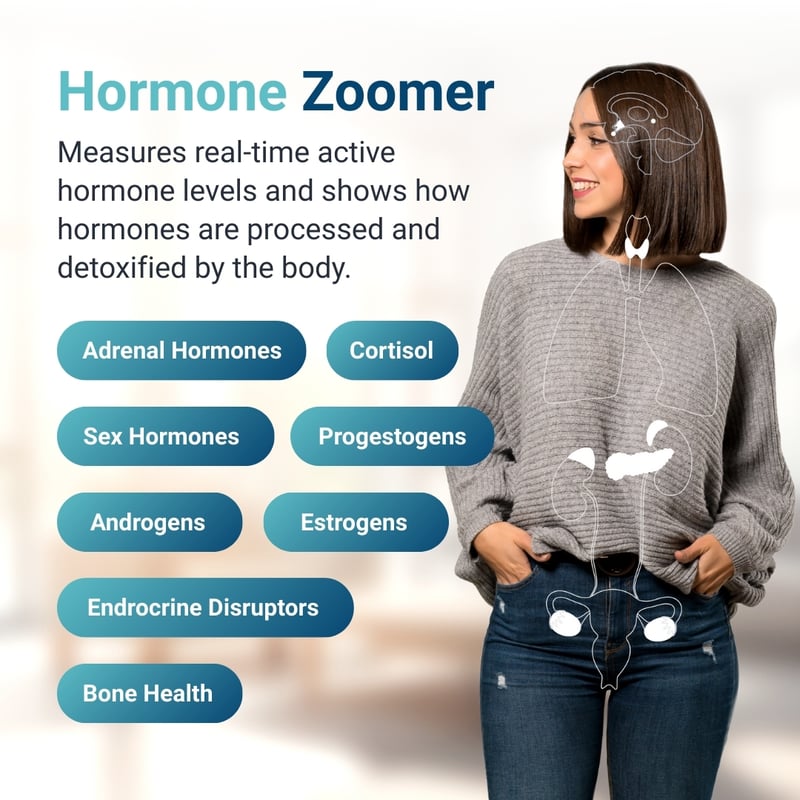
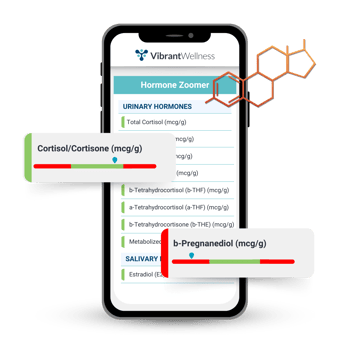
This article explores how dysregulation in estrogen, progesterone, cortisol, and thyroid hormones can contribute to autoimmune risk, and how integrative hormone testing and autoimmune disorder testing, like Vibrant’s Hormone Zoomer and Autoimmune Zoomer, can help providers uncover root drivers and tailor clinical strategies for lasting immune support.
Table of Contents
Clinical Application: Red Flags for Hormone-Immune Testing |
|
| Why Conventional Labs Often Miss the Full Picture
|
Key Takeaways |
About The Author
|
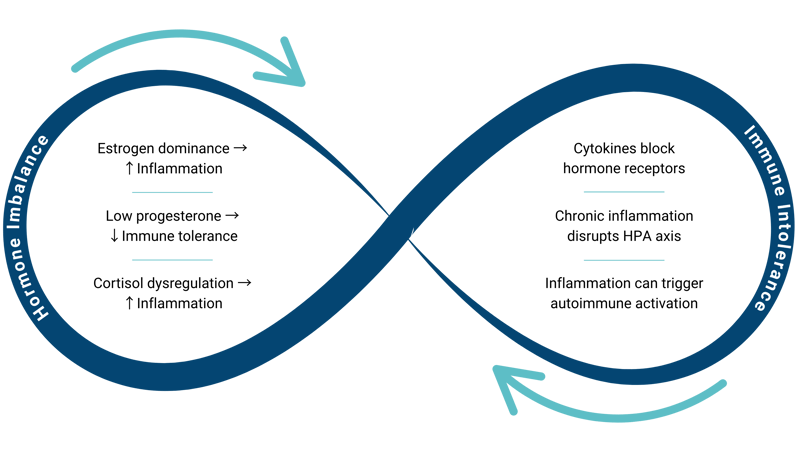
The Hormone-Immune Axis: A Bidirectional System
Hormones and immune cells operate in a dynamic feedback loop. This interaction, known as the hormone-immune axis, is a critical but often overlooked factor in immune regulation and autoimmune risk, particularly in women.
Hormone Imbalance and Inflammation

Immune cells express receptors for various hormones, including estrogen, progesterone, cortisol, and thyroid hormones. These hormones influence immune cell development, activation, and cytokine signaling.
- Sex hormones can promote either immune tolerance or activation, depending on the balance or timing.
- Glucocorticoids (like cortisol) act as powerful immunosuppressants that help control inflammation and prevent excessive immune responses.
Even subtle hormonal fluctuations can shift the immune system toward a pro-inflammatory or autoimmune-prone state, especially when compounded by stress, environmental exposures, poor nutrient intake, or gut dysbiosis.
Learn more about the relationship between the gut microbiome and hormone balance.
Immune Activation Alters Hormonal Balance
The feedback goes both ways. Chronic immune activation, common in autoimmunity, can impair hormone production and disrupt endocrine signaling through several mechanisms:
- Pro-inflammatory cytokines can interfere with hormone receptor expression and downstream signaling.
- Chronic inflammation disrupts the HPA axis, initially elevating cortisol levels, then leading to eventual depletion and poor stress resilience.
- Nutrient depletion impairs hormone synthesis (such as selenium for thyroid hormone, B6 for progesterone production, and magnesium for cortisol regulation).
The Vibrant Micronutrient Panel is a valuable tool for identifying these foundational nutrient gaps that weaken immune resilience and hormonal balance.
Why This Matters for Women
Women are particularly vulnerable to hormone-immune disruption during key life stages: from their first menstrual cycle to pregnancy, postpartum, and menopause. These hormonal shifts can tip the immune system toward intolerance and inflammation. For patients presenting with fatigue, joint pain, brain fog, or mood changes, the hormone-immune axis offers a powerful framework for root-cause investigation.
Key Hormones in Autoimmune Risk
Estrogen, progesterone, cortisol, and thyroid hormones all influence immune regulation. When these hormones become imbalanced—due to stress, life transitions, nutrient depletion, or environmental exposures—immune tolerance can break down, increasing the risk of autoimmune activation.
Estrogen’s Immune Impact: It’s Complicated
Estrogen plays a multifaceted role in immune regulation. It is generally immune-enhancing through its anti-inflammatory effects, but depending on timing, dose, and hormonal context, it can also act as an immunosuppressant. In some settings, estrogen promotes immune tolerance and dampens inflammation; in others, it stimulates immune activation and may contribute to autoimmunity.
These dual effects make estrogen a powerful but unpredictable player in immune health, which is why it’s valuable to track its patterns and metabolites through tools like the Hormone Zoomer.
Estrogen has been shown to:
- Influence innate immune cells like macrophages, potentially shortening the pro-inflammatory phase
- Inhibit pro-inflammatory cytokines such as IL-6 and TNF-α
- Modulate the NLRP3 inflammasome, either suppressing or promoting inflammation depending on the hormonal context
- Promote B cell activation and survival while interfering with the elimination of autoreactive B cells, increasing autoantibody risk
Women may become vulnerable to estrogen excess, deficiency, or abrupt withdrawal, particularly during puberty, perimenopause, and postpartum. The Hormone Zoomer helps clarify potential estrogen and immunity patterns by assessing multiple forms of estrogen, their metabolites, and environmental xenoestrogens that amplify immune activation.
Progesterone: The Unsung Regulator of Immune Tolerance
While estrogen can amplify immune responses, progesterone plays a calming, regulatory role, signaling immune cells to reduce inflammation and support repair. It's a critical modulator of immune tolerance, especially during hormonally dynamic life stages.
Key immunoregulatory actions of progesterone include:
- Activating regulatory T cells (Tregs) to prevent excessive inflammation
- Suppressing IL-6 and TNF-α, and downregulating the NF-kB pathway
- Inhibiting Th1 and Th17-driven immune responses linked to tissue damage
Whether during the luteal phase, postpartum, perimenopause, or chronic stress, declining progesterone removes this immune check and contributes to:
- Increased systemic inflammation
- Loss of immune tolerance
- Higher risk of autoimmune flares or disease onset
In early perimenopause, progesterone often drops while estrogen fluctuates, contributing to symptoms like heavy periods, headaches, mood shifts, and insomnia, alongside increased autoimmune risk. Functional hormone testing, like the Hormone Zoomer, helps assess progesterone metabolites and estrogen-progesterone ratios to guide hormone therapy decisions and ensure proper detoxification.
Cortisol: Stress, Inflammation, and Immune Regulation
Cortisol is a potent suppressor of inflammation, helping regulate immune responses during stress. But when cortisol becomes chronically elevated or depleted due to HPA axis dysfunction, immune regulation begins to break down.
cortisol becomes chronically elevated or depleted due to HPA axis dysfunction, immune regulation begins to break down.
Cortisol dysregulation may:
- Disrupt circadian rhythm, particularly when cortisol spikes late in the day, impairing restorative sleep and immune reset
- Lead to glucocorticoid resistance, where immune cells ignore cortisol’s regulatory signals
- Suppress T cell proliferation and activity
- Increase Th17-driven inflammation, implicated in autoimmune diseases such as RA, IBD, and psoriasis
Correcting cortisol curve imbalances is essential to restoring immune tolerance and reducing autoimmune flare risk. A bioavailable hormone test like Hormone Zoomer includes diurnal cortisol mapping and metabolite analysis for a complete picture of adrenal function. Meanwhile, the Autoimmune Zoomer identifies specific autoimmune markers early and accurately, enabling personalized treatment plans and improved patient outcomes.
Thyroid Hormones and Immune Function
There is growing evidence of direct crosstalk between thyroid hormones and the immune system. While the mechanisms are still being explored, thyroid hormones have been shown to:
mechanisms are still being explored, thyroid hormones have been shown to:
- Influence immune cells such as monocytes, NK cells, macrophages, and lymphocytes
- Support lymphocyte maturation and responsiveness
- Modulate cytokine production, especially via T3
Subclinical hypothyroidism (when TSH is normal but free hormones are low) can impair immune signaling and increase autoimmune risk. A full thyroid panel (TSH, Free T4, Free T3, Reverse T3, TPO antibodies, and thyroglobulin antibodies) along with nutrient evaluation (selenium, zinc, iron, and vitamin A) through the Micronutrient Panel provides a more complete picture.
Hashimoto’s thyroiditis, the most common autoimmune disease in women, often begins with vague symptoms like fatigue or brain fog, long before abnormal TSH appears. The Autoimmune Zoomer includes anti-TPO and anti-thyroglobulin antibodies to support earlier detection.
Why Conventional Labs Often Miss the Full Picture
Many women who feel tired, inflamed, or foggy are told their labs are normal. But “normal” doesn’t mean optimal, and traditional tests often overlook early dysfunction.
Gaps in Hormone Testing
Conventional hormone panels often miss critical insights because they:
- Use single-point measurements: This can be misleading due to daily fluctuations and individual variability.
- Exclude hormone metabolites: Without metabolite data, providers miss how hormones are being processed and cleared. This information is essential for understanding hormone burden and detox capacity.
- Miss hormonal rhythms: Hormones like cortisol follow a diurnal pattern. A single lab draw can miss curve flattening or late-day spikes that impact stress, sleep, and immune function.
Learn more about why understanding hormone health requires more than measuring hormone levels.
Gaps in Autoimmune Screening
Autoimmune tests also have limitations because they:
- Only detect disease once significant tissue damage has occurred
- Lack tissue specificity
- Fail to assess nutrient deficiencies contributing to immune deficiencies
What conventional labs miss, integrative hormone testing and autoimmune disorder testing may find.
Learn more about the role of sex hormones in autoimmunity.
The Benefits of Functional Testing
Functional testing can identify dysfunction earlier, allowing for proactive, personalized intervention. The following two tests can provide a clearer picture of hormone-immune dynamics and help tailor individualized support.
The Hormone Zoomer
The Hormone Zoomer assesses:
- Estrogen, progesterone, thyroid, and adrenal metabolites
- Detox pathways and endocrine disruptors
- Oxidative stress and bone health markers
This test helps link hormonal patterns to immune disruption, especially in perimenopause, postpartum, or stress states.
Autoimmune Zoomer
The Autoimmune Zoomer evaluates autoantibodies across 20+ systems:
- Thyroid, joints, pancreas, gut, and nervous system
- Early detection of tissue-specific immune reactivity
This test can be useful with vague, multi-system symptoms or a family history of autoimmunity.
Case Study: When “Normal” Isn’t Enough

Sarah, 44, presented with fatigue, worsening PMS, and joint pain. Routine labs—including TSH, estradiol, and a basic metabolic panel—were all within normal limits. But functional testing revealed several early imbalances, including:
- Low progesterone and impaired estrogen metabolism, consistent with estrogen excess and contributing to her PMS
- A flattened cortisol pattern, correlating with her persistent fatigue
- Early thyroid autoantibodies, potentially contributing to both fatigue and joint pain
Sarah’s care plan included progesterone replacement therapy, gut support, removal of endocrine-disrupting personal care products, stress reduction strategies, and targeted immune-supportive nutrients. Over time, Sarah’s symptoms improved, and she was able to intervene before autoimmunity progressed further.
Learn about the connection between perimenopause and autoimmunity.
Clinical Application: Red Flags for Hormone-Immune Testing
Consider running the Hormone Zoomer and Autoimmune Zoomer when patients present with:
- Persistent fatigue, joint pain, or brain fog with normal labs
- Worsening PMS or cycle changes, or symptoms of estrogen excess
- Postpartum symptoms that linger beyond the typical recovery window
- History of chronic stress, poor sleep, or flattened energy throughout the day
- Skin rashes, bloating, or unexplained food sensitivities
- Family history of autoimmune disease or personal history of multiple immune-related symptoms
- Major hormonal transitions or chronic stress
Testing during these windows allows providers to catch dysfunction early, identify immune or hormonal patterns that may be driving symptoms, and intervene before tissue damage occurs.
Key Takeaways
Hormonal shifts and immune dysregulation often go hand in hand, yet conventional testing rarely captures the complexity of that relationship. By integrating functional tools like the Hormone Zoomer and Autoimmune Zoomer, providers can identify subtle imbalances early and personalize care before inflammation progresses to chronic disease. For women navigating key life stages, this approach delivers clarity, early action, and lasting outcomes.
About the Author
Alison Bame, RD, CFMP, is a Registered Dietitian, Certified Functional Medicine Practitioner, and Hormone Expert specializing in women's health, midlife weight management, and autoimmune conditions. With over 15 years of experience, she helps women over 40 navigate perimenopause, hormonal imbalances, and metabolic challenges using a root-cause, functional medicine approach. A passionate educator and advocate for proactive healthcare, Alison empowers women to take charge of their health through personalized nutrition, hormone balance, and gut-immune support. Learn more about her work at AlisonBame.com.
Regulatory Statement:
The general wellness test intended uses relate to sustaining or offering general improvement to functions associated with a general state of health while making reference to diseases or conditions. This test has been laboratory developed and its performance characteristics determined by Vibrant America LLC and Vibrant Genomics, a CLIA-certified and CAP-accredited laboratory performing the test. The lab tests referenced have not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the test

Alison Bame, RD, CFMP

Find a Provider- Take Control of Your Health
Connect with a provider to access Vibrant Wellness specialty tests and personalized insights that support your long-term health.
Related Articles
If you’ve spent any time around teenagers, it might seem like they can deal with just about anything — crappy diets, late nights, emotional stress, and constant...

For women, menopause marks the end of reproductive capacity, but not the end of hormone activity. Once ovarian hormone production stops, the body depends on per...

For many women, the postpartum phase is physically exhausting and emotionally raw. And beneath the surface, the immune system is in flux, just like a house with...