When Hormone Cycles Collide with Autoimmunity
Understanding Menstrual-Driven Immune Flares and Clinical Testing Strategies
Many women with autoimmune conditions report that their autoimmune symptoms fluctuate throughout the month. Joint pain, fatigue, rashes, and mood shifts often intensify just before or during menstruation and, for some women, around ovulation.
Estrogen and progesterone aren’t just reproductive hormones. They’re immune modulators that affect inflammation, antibody production, and immune tolerance.
This article explores how menstrual cycle phases, hormonal imbalances (like estrogen dominance or luteal phase insufficiency), and synthetic hormones (such as those in contraceptives) can influence autoimmune flare-ups. We’ll also cover how clinicians can use the Hormone Zoomer and Autoimmune Zoomer to identify root causes, track patterns, and personalize treatment.
Table of Contents
How the Menstrual Cycle Shapes Immune Activity
While hormone fluctuations are a powerful trigger for autoimmune flares, they don’t act alone. Nutrient status, sleep quality, stress, physical activity, and exposure to toxins also play a role. Understanding how hormones fit into this broader picture enables more precise and proactive care.
The menstrual cycle isn’t just about reproduction. Each phase presents a distinct hormonal environment that influences how the immune system responds to internal and external stressors.
.png?width=1080&height=720&name=New%20Blog%20Post%20-%20Feature%20Image%20(15).png)
Follicular Phase (Day 1–13): Estrogen begins to rise as the uterine lining rebuilds and the ovarian follicle matures. During this time, increased cytokine activity recruits more macrophages to the vaginal and reproductive tract tissues than in the luteal phase.
Ovulation (Around Day 14): Estrogen peaks, triggering a surge in luteinizing hormone (LH). This phase can bring heightened immune activation, which for some women may trigger symptoms such as joint pain, rashes, or flares in conditions like lupus.
Luteal Phase (Day 15–28): Progesterone becomes the dominant hormone. It brings an immunosuppressive influence, calming immune responses and promoting tolerance.
Menses (Day 1 of the new cycle): A sudden drop in both estrogen and progesterone signals the shedding of the uterine lining. For some women, this hormone withdrawal leads to a flare in autoimmune symptoms like fatigue, migraines, or mood changes.
Hormones and the Immune System
Hormones don’t just fluctuate—they modulate the immune system.
- Estrogen enhances immune activity. It upregulates IL-4 and downregulates NF-kB, generally dampening inflammation. However, when levels are too high (or shift too quickly), it can overstimulate antibody production, thereby increasing the risk of autoimmune flares in susceptible individuals.
- Progesterone promotes immune tolerance. It supports the development of regulatory T cells (Tregs), modulates inflammatory cytokines, and helps the immune system distinguish friend from foe.
- Luteinizing hormone (LH) plays a role in regulating the immune system. LH can influence the number and activity of regulatory T cells (Treg). Tregs help regulate your body’s immune tolerance and response to prevent it from overreacting to harmful invaders, such as antigens.
When hormones become imbalanced or when hormone shifts are abrupt, women may become more susceptible to immune flares.
Common examples include:
- Hashimoto’s thyroiditis: Fatigue, brain fog, and mood symptoms often intensify before menstruation.
- Lupus (SLE): Many women experience skin or joint flares around ovulation.
- Rheumatoid arthritis: Flares frequently emerge during menses due to hormone withdrawal.
Key Insight: Many women feel “fine” during part of the month, then symptomatic again as hormone patterns shift. This cyclical fluctuation can mask chronic immune dysfunction, potentially delaying diagnosis or treatment.
Hormonal Imbalance: When Estrogen Outpaces Progesterone
Hormonal balance is essential for immune regulation. When estrogen levels exceed progesterone, whether due to anovulatory cycles, toxin exposure, or impaired detoxification, the result is often heightened inflammation and reduced immune tolerance. This estrogen excess can create fertile ground for autoimmune flares, especially in women with underlying susceptibility.

Causes of Excess Estrogen
- Anovulatory cycles (typical in adolescence, PCOS, perimenopause, or with hormone imbalances such as low FSH, LH, GnRH, or hypothyroidism) result in no ovulation, and therefore no progesterone to counterbalance rising estrogen levels.
- Xenoestrogens, found in many personal care and household products (like phthalates, parabens, and BPA), mimic estrogen in the body and bind to receptors with exaggerated, prolonged effects.
- Obesity, particularly central adiposity, increases estrogen production via adipose tissue and elevates inflammatory cytokines that can further disrupt hormone balance.
- Poor detoxification due to sluggish liver pathways, constipation, or elevated beta-glucuronidase activity impairs estrogen clearance, allowing the reabsorption of estrogen metabolites that can activate the immune system.
Why Progesterone Matters For Immune Health
Progesterone is produced by the corpus luteum after ovulation, which means it is only made when ovulation occurs. While its most well-known role is supporting pregnancy, progesterone has powerful whole-body effects that are especially relevant for autoimmune health.
- Balances estrogen’s stimulating effects, helping to maintain immune tolerance
- Helps regulate the nervous system, enhancing the body’s ability to manage stress
- Supports thyroid function by sensitizing tissues to thyroid hormone
- Protects cardiovascular health by relaxing smooth muscle and reducing vascular inflammation
- Promotes restorative sleep, a vital component of immune regulation and flare prevention
- Supports lean muscle mass, which is key to metabolic and inflammatory balance
Clinical Conditions Linked to Low Progesterone
When progesterone is consistently low, whether due to anovulation, chronic stress, perimenopause, or other hormonal imbalances, women may experience a wide range of symptoms and conditions, including:
- PCOS, endometriosis, and autoimmune conditions
- PMS, fibroids, mood changes, and acne
- Perimenopause and menopause-related symptoms
- Infertility and early pregnancy loss
- Osteoporosis and low bone density
- Premenstrual migraines
Even when ovulation occurs, there are situations where the corpus luteum produces insufficient progesterone, a condition known as luteal phase insufficiency.
Physical Signs of Luteal Phase Insufficiency
- A short luteal phase (less than 11 days)
- Low temperatures during the luteal phase (via basal body temperature tracking)
- Presence of fertile cervical mucus after ovulation
- Premenstrual spotting
Hormonal Contraceptives and Immune Disruption
How do hormonal birth control options affect autoimmunity? The answer is complex, and further research is needed.
A primary mechanism behind these effects is the suppression of ovulation and endogenous hormone production.
Most hormonal contraceptives, including pills, implants, and injections, work by suppressing ovulation and halting the natural production of estradiol and progesterone. While this method is effective in preventing pregnancy, it also eliminates the immune-regulating benefits of these natural hormones. It alters hormone-immune signaling in ways that may contribute to immune dysregulation.

Research Highlights and Risks
A large hormonal contraceptive and autoimmunity review concluded that hormonal contraceptives modulate immune function and are associated with increased risk for several autoimmune diseases:
- Combined oral contraceptives are linked to:
- Increased risk of lupus, Crohn’s disease, ulcerative colitis, multiple sclerosis, and interstitial cystitis
- A lower incidence of hyperthyroidism in some cases
- Elevated C-reactive protein, a marker of systemic inflammation.
- Progestin-only contraceptives (including implants, mini-pills, and some IUDs):
- Have been shown to increase inflammatory cytokines in some studies
- May bind to multiple hormone receptors (not just the progesterone receptor), including glucocorticoid, mineralocorticoid, androgen, and possibly the estrogen receptors
- May worsen mood, reduce stress resilience, and interfere with immune responses in susceptible individuals
Hormonal IUDs contain synthetic progestins and may suppress ovulation, especially during the initial months of use. However, ovulation may resume over time, depending on the individual and duration of use.
Contraceptive Counseling in Autoimmune-Prone Patients
- Ask autoimmune-prone patients about their current and past contraceptive history.
- Consider non-hormonal alternatives (such as copper IUDs, barrier methods, or fertility awareness method - FAM) when appropriate.
- If hormonal contraception is necessary, proactively support liver detoxification, gut health, and micronutrient status to reduce immune burden.
Hormonal birth control is not the root cause of autoimmunity, but it may tip the balance in a susceptible individual.

Clinical Assessment Strategies
How do I test for this in practice?
Fortunately, there are tools that, when used together, help connect immune flare patterns to hormonal imbalances and give you a personalized roadmap for support.
Urinary Hormone Testing
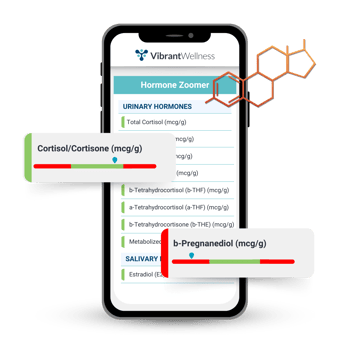 The Hormone Zoomer offers a more nuanced view than standard serum hormone panels. Rather than just measuring what’s circulating in the blood, it reveals what the body is using at the tissue level.
The Hormone Zoomer offers a more nuanced view than standard serum hormone panels. Rather than just measuring what’s circulating in the blood, it reveals what the body is using at the tissue level.
What the Hormone Zoomer can identify:
- Estrogen excess (compared to progesterone) or poor estrogen detoxification
- Luteal phase insufficiency (low progesterone production)
- Cortisol patterns that reflect HPA axis stress
- Burden of endocrine disruptors like BPA, phthalates, and parabens
Why this matters: These insights help explain why symptoms flare during certain phases of the cycle and offer clear targets for intervention, whether that’s improving detox pathways, supporting ovulation, or calming cortisol output.
Autoimmune Testing
The Autoimmune Zoomer detects early immune reactivity and helps track antibody progression across time.
This test screens for:
- Organ-specific autoantibodies across systems (thyroid, joints, gut, skin, brain, etc.)
- Antibody patterns that may correlate with symptom timing
- Signs of immune hyperactivity that may be influenced by hormone shifts
Cycle Symptom Tracking
Some of the most valuable data still comes directly from the patient. Encourage women to track their cycle alongside their symptoms (energy levels, joint pain, migraines, mood changes, and more).
Apps, journals, or a simple paper tracker can help identify:
- When flares occur
- Whether they align with ovulation, luteal drop-off, or menses
- Signs of luteal phase insufficiency or anovulatory cycles
- Lifestyle contributors (such as stress, sleep, and nutrition) that may be influencing symptoms
When paired with testing, this approach empowers both the clinician and the patient to spot trends, adjust support plans, and measure progress over time.
Case Study: Connecting Hormones and Flares in a Hashimoto’s Patient
Patient Presentation
A 35-year-old woman with Hashimoto’s thyroiditis presented with persistent fatigue, brain fog, and monthly migraines that intensified in the week before her period. She also reported worsening PMS symptoms and difficulty maintaining consistent energy.
-1.png?width=1080&height=405&name=2024%20-%20A%20Comprehensive%20Approach%20to%20Recurrent%20UTIs%20(6)-1.png)
Testing Insights
- Hormone Zoomer showed low progesterone, elevated estrogen metabolites, and signs of poor methylation capacity.
- Autoimmune Zoomer revealed rising thyroid antibody levels compared to earlier panels.
These findings pointed toward insufficient progesterone following ovulation and impaired estrogen clearance, both of which can tip the immune system toward flare activity.
Targeted Interventions
- Introduced Vitex to support ovulation and endogenous progesterone production.
- Added DIM to aid estrogen detoxification.
- Switched her multivitamin to one with methylated B vitamins and trimethylglycine to support methylation
- Targeted immune and thyroid support with zinc, vitamins A and D, adequate protein, iodized salt, and Brazil nuts (as a selenium source).
- Focused on lifestyle foundations, including consistent movement and improving sleep hygiene, especially in the luteal phase
Patient Outcomes
Within three months, the patient reported more stable energy, fewer migraines, lighter, more predictable cycles, and a significant reduction in premenstrual flares.

Next Steps for Cycle-Aware Autoimmune Care
Hormonal shifts are only one piece of the autoimmune puzzle, but they’re a piece worth paying attention to, especially when flares follow a cyclical pattern. By pairing symptom tracking with targeted testing, clinicians can begin to see meaningful patterns that inform more personalized care.
Key considerations for clinical practice:
- Check hormone balance with a focus on estrogen & progesterone metabolism, and detoxification patterns.
- Track autoantibodies to monitor disease progression and identify potential flare patterns.
- Support immune resilience by evaluating and addressing other foundational factors like nutrient status, gut health, chronic stress, toxin exposures, and sleep quality.
Autoimmune diseases may not be curable, but they are manageable. Understanding how hormones fit into the larger picture helps clinicians deliver care that’s proactive, precise, and better aligned with each woman’s unique physiology.
About the Author
Alison Bame, RD, CFMP, is a Registered Dietitian, Certified Functional Medicine Practitioner, and Hormone Expert specializing in women's health, midlife weight management, and autoimmune conditions. With over 15 years of experience, she helps women over 40 navigate perimenopause, hormonal imbalances, and metabolic challenges using a root-cause, functional medicine approach. A passionate educator and advocate for proactive healthcare, Alison empowers women to take charge of their health through personalized nutrition, hormone balance, and gut-immune support. Learn more about her work at AlisonBame.com.
Regulatory Statement:
The information presented in case studies have been de-identified in accordance with the HIPAA Privacy protection. The general wellness test intended uses relate to sustaining or offering general improvement to functions associated with a general state of health while making reference to diseases or conditions. This test has been laboratory developed and its performance characteristics determined by Vibrant America LLC and Vibrant Genomics, a CLIA-certified and CAP-accredited laboratory performing the test. The lab tests referenced have not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the test.

Alison Bame, RD, CFMP

Find a Provider- Take Control of Your Health
Connect with a provider to access Vibrant Wellness specialty tests and personalized insights that support your long-term health.
Related Articles
If you’ve spent any time around teenagers, it might seem like they can deal with just about anything — crappy diets, late nights, emotional stress, and constant...

Nearly 80% of people with an autoimmune disease are women. This striking statistic underscores the need to examine the potential connection between hormone imba...

For many women, the postpartum phase is physically exhausting and emotionally raw. And beneath the surface, the immune system is in flux, just like a house with...