How Heavy Metals Worsen Neuroinflammation and Mast Cell Dysfunction
The Hidden Neuroimmune Impact of Toxic Metals
Every day, we're exposed to trace amounts of heavy metals: arsenic in drinking water, mercury in seafood, lead in old pipes, cadmium in air pollution, and tobacco smoke. While these exposures may seem inconsequential, a growing body of research suggests otherwise.
Chronic, low-level accumulation of these metals can profoundly affect the immune and nervous systems in ways that are often overlooked in standard clinical assessments. The combined activation of mast cells and microglia by heavy metals is a potent driver of neurological symptoms such as brain fog, anxiety, and fatigue.
Despite the clear mechanistic links and emerging clinical data, toxic metals remain an underappreciated root cause of chronic illness. This article explores how heavy metals ignite mast cell activation and microglial inflammation, how these mechanisms drive neuroimmune dysregulation, and how functional testing for heavy metal exposure can help you uncover, and address, this hidden source of disease in your patients.
Table of Contents
Mast Cell Activation and Toxins: Hidden Dangers of Heavy Metal Exposure
Heavy metals such as mercury, lead, cadmium, and arsenic are widely recognized for their neurotoxic effects, but their impact extends far beyond direct neuronal damage. Mounting research shows that these metals can activate mast cells and microglia, two sentinel immune cells that sit at the interface of the nervous and immune systems and serve as the brain’s early warning system. This activation can trigger neuroinflammation, oxidative stress, and downstream neuroimmune dysfunction.
Mast cells are exquisitely sensitive to environmental stimuli, including toxicants, and play a central role in initiating inflammatory responses. Microglia, the resident immune cells of the brain, become activated in response to these signals and orchestrate a cascade of neuroimmune activity. The crosstalk between these cells is a crucial link in the chain of events that transforms toxic exposures into neurological symptoms. (Skaper et al., 2012; Zhang et al., 2016).
![]()
Research shows that environmental toxins such as arsenic can disrupt glial function and contribute to the breakdown of the blood-brain barrier, resulting in neuroinflammation and neuronal injury (Bandyopadhyay & Shukla, 2023). Heavy metals are also known to induce mitochondrial dysfunction, deplete antioxidant reserves, and alter immune signaling pathways like NF-κB and AP-1, all of which amplify inflammatory responses (Korashy et al., 2008; Karri et al., 2016).
How Heavy Metals Worsen Neuroinflammation and Cellular Dysfunction
Mast cells, which are positioned at barrier sites like the gut and blood-brain barrier, are highly sensitive to heavy metal exposure. Metals like mercury and cadmium have been shown to stimulate mast cell degranulation, increasing the release of inflammatory mediators such as histamine, IL-4, and TNF-α (Suzuki et al., 2011; Dastych et al., 1999). These toxic metals can also disrupt redox signaling, enhance calcium influx, and activate downstream pathways like NF-κB, further amplifying cytokine production and inflammation (Chen & Shi, 2002; Suzuki et al., 2005).

Microglia, the resident immune cells of the brain, also respond to heavy metal exposure by shifting into an activated, pro-inflammatory state. For instance, cadmium and lead exposure can induce morphological and metabolic changes in microglia, stimulate the release of pro-inflammatory cytokines, and disrupt mitochondrial function (Bovio et al., 2023; Liu et al., 2015). These changes may compromise blood-brain barrier integrity, promote oxidative stress, and initiate a feedback loop that exacerbates neuroinflammation (Bandyopadhyay & Shukla, 2023).
Critically, mast cells and microglia communicate and co-activate in response to environmental stimuli. Activated mast cells can trigger microglial activation via the release of histamine, prostaglandins, and protease-activated receptor ligands (Zhang et al., 2016). This bidirectional crosstalk has been shown to contribute to the development of neurodegenerative diseases and increase neuroimmune dysfunction in the presence of toxicants (Skaper et al., 2017; Skaper et al., 2012).
Clinically, the symptoms of heavy metal neurotoxicity can be vague and varied, ranging from brain fog and fatigue to anxiety, insomnia, and histamine intolerance (Gui et al., 2023; Mason et al., 2013; Mfem et al., 2021). In some cases, lead or mercury brain inflammation can even masquerade as psychiatric or neurodegenerative conditions such as depression, Parkinson’s disease, or early-onset dementia (Chang et al., 2015; Kern et al., 2014).
The effects may be even more pronounced in individuals with underlying sensitivity or impaired detoxification capacity. As such, understanding these immune mechanisms is essential when evaluating patients with chronic neuroinflammatory presentations and unexplained toxic burden.
Mitochondrial Damage and Oxidative Stress: The Central Nexus
 One of the most damaging downstream effects of heavy metal exposure is mitochondrial dysfunction, particularly within energy-demanding and immune-responsive tissues like the brain. Mercury, cadmium, lead, and arsenic are all known to impair mitochondrial bioenergetics by disrupting the electron transport chain, generating reactive oxygen species (ROS), and compromising membrane integrity (Sun et al., 2022; Cheng et al., 2021). These disruptions inhibit ATP synthesis and initiate apoptotic cascades, ultimately leading to neurodegeneration and immune dysregulation (Korotkov, 2023; Agnihotri et al., 2019).
One of the most damaging downstream effects of heavy metal exposure is mitochondrial dysfunction, particularly within energy-demanding and immune-responsive tissues like the brain. Mercury, cadmium, lead, and arsenic are all known to impair mitochondrial bioenergetics by disrupting the electron transport chain, generating reactive oxygen species (ROS), and compromising membrane integrity (Sun et al., 2022; Cheng et al., 2021). These disruptions inhibit ATP synthesis and initiate apoptotic cascades, ultimately leading to neurodegeneration and immune dysregulation (Korotkov, 2023; Agnihotri et al., 2019).
As well as being the powerhouses of the cell, mitochondria are regulators of redox homeostasis. Heavy metals interfere with antioxidant enzyme systems, such as glutathione peroxidase and superoxide dismutase, resulting in excessive ROS production and oxidative stress (Ghasemi et al., 2014; Balali-Mood et al., 2021). This oxidative burden damages lipids, proteins, and DNA within neural and immune cells, weakening cellular resilience and fueling chronic inflammation (Rubino, 2015; Farina et al., 2013).
 Moreover, heavy metals can deplete glutathione, a master intracellular antioxidant, by binding to thiol groups or interfering with glutathione synthesis and recycling (Ercal et al., 2001; Flora et al., 2008). In some cases, metals like mercury directly inhibit mitochondrial complex activity or trigger calcium overload, leading to mitochondrial swelling and membrane permeabilization (Belyaeva et al., 2011; Karri et al., 2016). These structural insults further limit a cell’s ability to detoxify and recover from oxidative stress.
Moreover, heavy metals can deplete glutathione, a master intracellular antioxidant, by binding to thiol groups or interfering with glutathione synthesis and recycling (Ercal et al., 2001; Flora et al., 2008). In some cases, metals like mercury directly inhibit mitochondrial complex activity or trigger calcium overload, leading to mitochondrial swelling and membrane permeabilization (Belyaeva et al., 2011; Karri et al., 2016). These structural insults further limit a cell’s ability to detoxify and recover from oxidative stress.
In mast cells and microglia, mitochondrial impairment can exacerbate immune hyperreactivity and prolong the inflammatory response. By disrupting energy metabolism and antioxidant defenses in these immune cells, heavy metals promote a state of unresolved inflammation that contributes to neuroimmune dysregulation and chronic symptoms such as fatigue, brain fog, and heightened chemical sensitivity.
Clinically, this mechanistic insight reinforces the importance of testing for mitochondrial stress markers and antioxidant status, particularly in individuals with a known or suspected toxicant burden. Tests such as Vibrant’s Oxidative Stress Profile and NutriPro Panel can be instrumental in identifying redox imbalances and guiding targeted antioxidant support.
Functional Testing To Guide Detoxification and Recovery
Uncovering the root causes of neuroinflammation and mast cell activation requires a comprehensive view of toxicant burden and metabolic resilience. Functional testing provides the clinical clarity needed to guide detoxification strategies and nutrient support tailored to each patient’s biochemical profile.
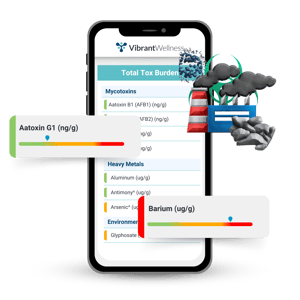 Vibrant’s Total Tox Burden panel is an ideal starting point. This advanced urine-based test assesses 87 different toxicants across three categories, including heavy metals, mycotoxins, and environmental chemicals.
Vibrant’s Total Tox Burden panel is an ideal starting point. This advanced urine-based test assesses 87 different toxicants across three categories, including heavy metals, mycotoxins, and environmental chemicals.
It quantifies individual exposures to metals like mercury, lead, cadmium, and arsenic, while also revealing the cumulative toxicant load that may be impairing immune, neurological, and mitochondrial function. This panel is especially useful for patients with unexplained fatigue, chemical sensitivities, histamine intolerance, or neuropsychiatric symptoms that don’t resolve with standard interventions.
To further personalize care, pairing the Total Tox Burden with the NutriPro Panel can reveal critical micronutrient depletion from toxic metals and genetic variants that impact detoxification capacity. For instance, deficiencies in selenium, zinc, and B vitamins are commonly associated with greater vulnerability to metal-induced oxidative stress and glutathione depletion (Rahman et al., 2019; Gałażyn-Sidorczuk et al., 2012). Testing for these nutrients offers insight into a patient’s ability to mount an antioxidant response and restore redox balance during detox protocols for heavy metals.
Additionally, the Oxidative Stress Profile can identify real-time evidence of redox imbalance by measuring biomarkers of lipid peroxidation, DNA damage, and protein oxidation. Markers like 8-OHdG, 8-iso-PGF2α, and dityrosine provide a snapshot of the oxidative damage that may be driving neuroinflammation and immune dysfunction.
For patients presenting with neurological symptoms, integrating the Neural Zoomer Plus may help identify antibodies to neural antigens, offering insight into potential autoimmune or inflammatory processes impacting the brain. While heavy metals themselves are not always directly implicated in antibody production, their role in priming immune activation and neurotoxicity can create the conditions under which autoimmunity develops or worsens.
Together, these panels allow clinicians to move beyond symptom management and begin connecting environmental triggers to physiological dysfunction. Testing becomes the foundation for a functional strategy that includes reducing exposure, supporting detox pathways, and replenishing depleted nutrients, all while tracking progress through repeat assessments.
Connecting the Dots: Case-Based Clinical Integration
Consider a 42-year-old woman presenting with persistent brain fog, histamine intolerance, fatigue, and increasing chemical sensitivity. Despite clean labs, a nutrient-dense diet, and previous success with gut-focused protocols, her symptoms persist.
She works in a hospital environment and reports childhood exposure to well water, both potential sources of chronic low-grade heavy metal accumulation. In cases like this, functional testing becomes essential.

Her Total Tox Burden reveals elevated urinary mercury and cadmium. The NutriPro Panel shows low levels of selenium and zinc, along with reduced B12 and glutathione activity, factors that compromise metal clearance and antioxidant defenses.
Her Oxidative Stress Profile flags elevated 8-iso-PGF2α, suggesting active lipid peroxidation. While her Neural Zoomer Plus does not indicate autoantibodies, her neuroinflammatory symptoms, particularly fatigue and sensory sensitivity, align with known effects of toxicant-induced mast cell and microglial activation (Šterzl et al., 1999; Dike et al., 2023).
This patient's presentation reflects the growing number of patients who exhibit MCAS-like symptoms, neuroinflammation, and vague chronic illness due to environmental xenobiotic overload. Evidence suggests that metals like mercury, cadmium, and lead may provoke mast cell mediator release and microglial activation, especially in genetically susceptible individuals (Miller et al., 2021; Hemdan et al., 2007). This immune sensitization may occur in parallel with metabolic disruptions such as mitochondrial dysfunction, glutathione depletion, and altered Th1/Th2 balance (Patrick, 2002; Planchart et al., 2018).
Once toxicant burden is identified, the clinical roadmap shifts toward detoxification and immune modulation. First, address re-exposure risks through environmental hygiene, dental material review, and filtered water.
Next, implement foundational detox support including phase I and II liver cofactors, B vitamins, magnesium, selenium, and glycine, as well as mast cell stabilizers like quercetin and DAO cofactors (Sears, 2013; Flora, 2009). Clinicians may also consider antioxidant chelators such as N-acetylcysteine or alpha-lipoic acid to support glutathione synthesis and metal mobilization (Bjorklund et al., 2019; Shay et al., 2009).
As recovery progresses, patients often report improved cognition, reduced histamine symptoms, and more stable mood and energy. Periodic retesting of toxicant and nutrient panels can guide the titration of protocols, reinforce compliance, and mark tangible milestones in healing.
Why Testing Is the First Step Toward Healing
Heavy metal exposure is not just a theoretical risk; it is a clinically relevant driver of neuroimmune dysfunction, oxidative stress and cognitive symptoms, and persistent inflammation. Mercury, lead, cadmium, and arsenic can bioaccumulate in tissues and silently disrupt the body’s most fundamental systems: energy metabolism, immune regulation, and neurological resilience. For patients with symptoms such as brain fog, anxiety, fatigue, histamine intolerance, or chemical sensitivity, these toxicants may be the missing link in an otherwise thorough functional assessment.
 Because of the bioindividual nature of detoxification and immune response, functional testing is essential for precision-guided intervention. Tests like Vibrant's Total Tox Burden panel quantify toxicant load to empower clinicians to remove exposure sources and initiate targeted support. Complementary panels such as NutriPro, Oxidative Stress, and Neural Zoomer Plus can help reveal the downstream impacts of heavy metals on antioxidant status, immune signaling, and neuroinflammation, enabling a systems biology approach to healing.
Because of the bioindividual nature of detoxification and immune response, functional testing is essential for precision-guided intervention. Tests like Vibrant's Total Tox Burden panel quantify toxicant load to empower clinicians to remove exposure sources and initiate targeted support. Complementary panels such as NutriPro, Oxidative Stress, and Neural Zoomer Plus can help reveal the downstream impacts of heavy metals on antioxidant status, immune signaling, and neuroinflammation, enabling a systems biology approach to healing.
These tools not only measure dysfunction but provide a roadmap for recovery. With this data in hand, clinicians can support detoxification through nutrient repletion, lifestyle strategies, and phase-specific protocols tailored to each patient’s biochemical individuality. In doing so, we move beyond symptom suppression and into true systems-based care, supporting the body’s innate capacity to heal, regulate, and defend.
When it comes to environmental toxicants, testing is not optional; it is foundational. Only by identifying and understanding the burden each patient carries can we begin to unburden their physiology, optimize their resilience, and move them toward lasting health.
About the Author
Brendan Vermeire is a Mental and Metabolic Health Scientist, Functional Medicine Educator, and Board-Certified Holistic Health Practitioner. After an injury ended his Navy SEAL training, he shifted to personal training, discovered functional lab testing, and became a leading expert in metabolic health. He founded the Metabolic Solutions Institute and its nonprofit arm, dedicated to advancing mental health science. He also created The Mental M.A.P.™ lab panel, the FMHP™ Certificate Program, and the NeuroCeuticals™ supplement line.
Regulatory Statement:
The information presented in case studies have been de-identified in accordance with the HIPAA Privacy protection.
The general wellness test intended uses relate to sustaining or offering general improvement to functions associated with a general state of health while making reference to diseases or conditions. This test has been laboratory developed and its performance characteristics determined by Vibrant America LLC and Vibrant Genomics, a CLIA-certified and CAP-accredited laboratory performing the test. The lab tests referenced have not been cleared or approved by the U.S. Food and Drug Administration (FDA). Although FDA does not currently clear or approve laboratory-developed tests in the U.S., certification of the laboratory is required under CLIA to ensure the quality and validity of the test.

Brendan Vermeire

Find a Provider- Take Control of Your Health
Connect with a provider to access Vibrant Wellness specialty tests and personalized insights that support your long-term health.
Related Articles
Autoimmune brain disorders represent one of the most complex and misunderstood intersections of neurology and immunology. Conditions such as multiple sclerosis ...

When most people think of histamine, they picture allergy symptoms, sneezing, hives, and congestion. But histamine is far more than an allergy molecule. It is a...

How do we get exposed to heavy metals? Many people consider heavy metal exposure to be rare, but sources of exposure are actually quite common. [1]